
Ophthalmologic examination may be within normal limits in asymptomatic or pre-symptomatic patients with NMOSD. Later, more suggestive and specific signs and symptoms of NMO may start to develop including optic neuritis or myelitis. Interestingly, patients can initially present with an acute flu-like illness (fever, myalgia, and headache). His case reports were vague and no pathology was documented Almost 80 years later, Stansbury published a thorough review on NMO and afterwards accepted as a separate entity from MS. The first association between myelitis and optic nerve disorder was reported in 1870 by Sir Thomas Clifford Allbutt. There are still unknown elements in the pathophysiology of NMOSD including the mechanism for loss of tolerance and anti-AQP4 formation, pathogenesis of seronegative NMOSD, and the mechanisms that anti-AQP4 breach the blood brain barrier. The loss of AQP4 immunoreactivity and the astrocyte pathology in the brain and spinal cord lesions distinguish NMOSD lesions from multiple sclerosis (MS) lesions. Local CNS water imbalance results in oligodendrocyte damage and demyelinization. Death of astrocytes induces secondary death of oligodendrocytes, resulting in demyelination and ultimately neuronal cell death. The proposed pathophysiology involves anti-AQP4 autoantibodies that are peripherally produced entering the CNS and binding astrocyte foot processes, which then induces complement mediated cell damage, granulocyte infiltration, and astrocyte death. AQP4 rich areas of the CNS account for the clinical findings of NMOSD. The AQP4 water channel membrane protein is concentrated in the optic nerve, area postrema, and spinal cord. NMO is characterized by a disease specific IgG antibody against the astrocytic aquaporin 4 (AQP4) water channel (also known as the aquaporin-4 autoantibody (anti-AQP4 or AQP4-IgG). The pathophysiology of NMOSD mainly involves the humoral immune system. Necrosis in NMOSD usually involves both gray and white matter, which is distinct from multiple sclerosis.
NMOSD produces significant axonal loss associated with perivascular lymphocytic infiltration and vascular proliferation.

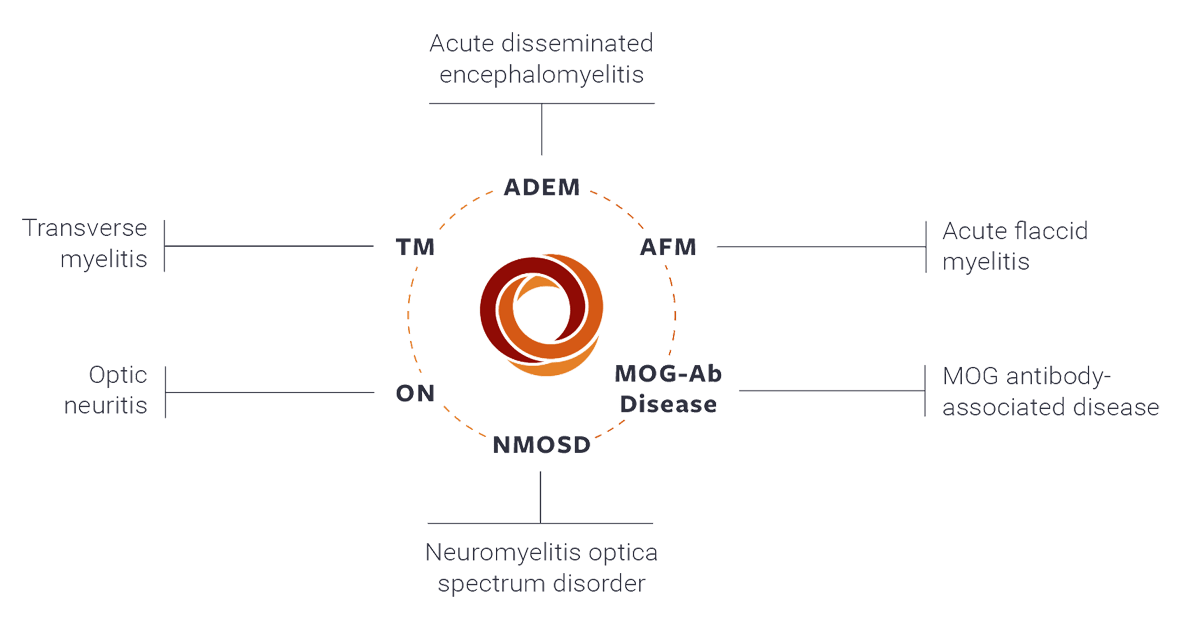
It involves demyelination and inflammation of multiple spinal cord segments and the optic nerves. NMO is characterized by segmented demyelination and inflammation of the spinal cord and the optic nerves inducing axonal loss and perivascular lymphocytic infiltration. Risk FactorsĪlthough NMOSD can occur in any ethnicity, either gender, and any age, the disease has a predilection for females and may be more common in patients of Asian or African descent. In the past there was debate as to whether NMO represented a variant of multiple sclerosis (MS), recent evidence however suggests that NMOSD has a completely different pathogenesis, pathology, mechanism of disease, presentation, course, treatment, and prognosis than MS. The precise etiology of NMOSD remains to be completely defined. Neuromyelitis optica (NMO) is an inflammatory disease that causes demyelination of the central nervous system, primarily affecting the optic nerve (optic neuritis) and the spinal cord.


 0 kommentar(er)
0 kommentar(er)
